-
-
-
-
URL copied!
Making the case for more efficient pre-authorization
The concept of authorization in the U.S. healthcare market is not a new one. However, the process itself has not yet matured and there is plenty of opportunity for improvements in automation and technology.
Authorization is a process whereby a provider submits a request to ensure that any given medical treatment is covered by the insurance company. This enables insurance companies to manage costs and provide their patients with higher quality care. It also helps to regulate the value-based care initiatives rendered by providers.
There are two main types of authorization.
Prior or Pre-Authorization: The healthcare provider obtains approval for the patient’s services prior to their being rendered. This happens in the majority of authorization-seeking cases. Learn more about prior authorization in this resource from America’s Health Insurance Plans (AHIP).
Retro Authorization: In rare exception cases and emergencies where pre-authorization is not possible, retro authorization may be requested from the insurance company after the patient’s treatment has been provided.
Payers are increasingly moving towards the automated and more regulated pre-authorization model, enabling them to optimize healthcare costs by approving requests within a quick turnaround time when all criteria are met. However, newly introduced protocols are putting more burden on the providers. In some cases, patients worry that pre-authorization creates delays rather than moving the process forward.
The healthcare industry was at the forefront of the pandemic and as such, had the greatest need for quick, digitized solutions with lower overhead to manage volume at the height of the crisis.
Some insurers were forced to temporarily suspend some pre-authorization requirements as the pandemic made it even more difficult to process paperwork in a timely way. These are among the reasons the healthcare industry has felt the pressing need for quick, adaptable pre-authorization solutions.
Pain Points with the Current Pre-authorization Process
There are several issues with the current pre-authorization process that make it more cumbersome and time-consuming than is ideal.
Approximately 66% of prescriptions rejected at the pharmacy require prior authorization, resulting in nearly 30% of these prescriptions being abandoned by patients. The reality that it takes 5-10 days for the insurance company to approve an authorization request can also delay procedures that can result in longer times to diagnosis, as well.
Further, the prior authorization physician survey conducted by the American Medical Association in December 2020 found that 69% of practicing physicians reported their health insurers had either reverted to pre-pandemic pre-authorization policies or never relaxed these policies in the first place. Only 1% of responding physicians said their health insurers maintained relaxed requirements through the end of 2020 when the U.S. health system was buckling under the strain of record numbers of COVID-19 cases.
There are several other issues with pre-authorization process problems that prevent it from being a smooth process.
It’s a Cumbersome Process for Providers
- Much time is wasted in providing information to the payers with too many manual interventions in the process.
- There is no clear picture for providers on which medical procedures need immediate attention for pre-authorization and which do not.
Patient Care May Be Delayed
- The real impact of delayed care is felt by patients who don’t get their medication or treatment on time.
- With delayed processing of pre-authorization requests and responses, claim requests may be denied due to incorrect information.
Lack of Standardization in Payer Rules for Various Insurance Plans
- Even though many rules have been rolled out by Centre for Medicare and Medicaid Services (CMS), many insurance companies still follow different processes with varying rules on how to intake the pre-authorization request from the provider and process it further into the system.
- There are no set rules and standards yet that are being followed across every payer.
Manual Interventions
- Pre-authorization via faxes and paper forms needs a lot of manual intervention before the request can be processed accurately within the system.
New CMS Guidelines for Pre-authorization
In Dec 2020, CMS proposed new (final) rules to help streamline the pre-authorization process. These are designed to bring consistency and transparency to the API and services so end-users can make the right decisions and achieve better outcomes.
Organizations building solutions in keeping with these new rules can incorporate these features:
- Medicaid, CHIP, and QHP payers will be required to build APIs that can enable and streamline data processing. Medicare Advantage Plans are currently excluded from this rule.
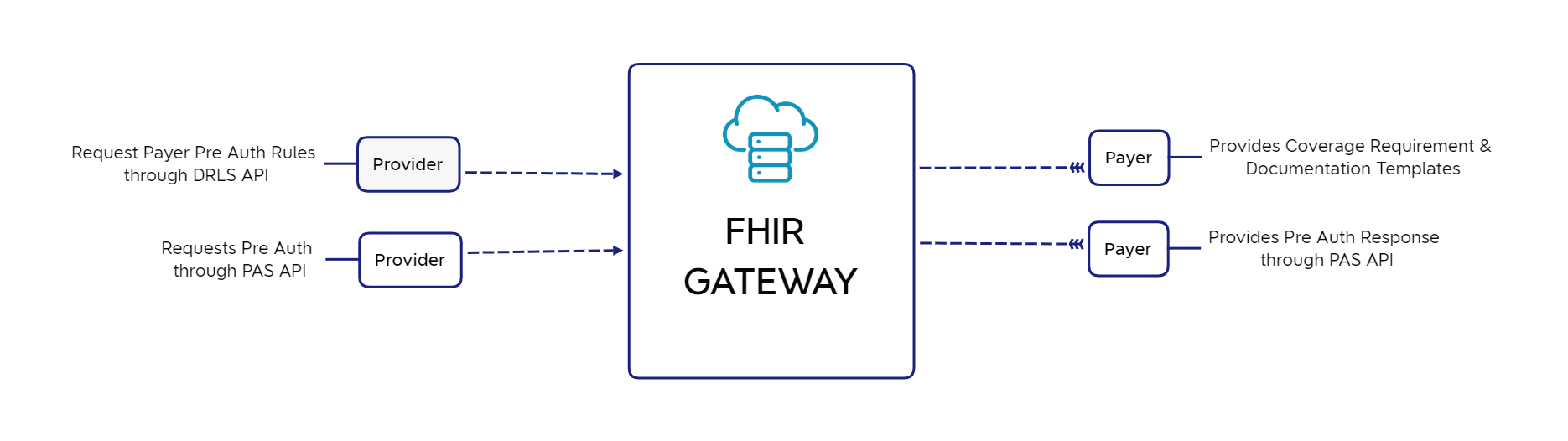
- Providers will be able to electronically inquire about Pre-Auth requirements for a specific payer and items/services.
- Providers will be able to electronically submit Pre-Auth Requests and receive acknowledgment (in coordination with existing HIPAA X12 transactions).
- System integrations should support electronic status updates for the case/claim, as per the API standards.
- There should be an ability to provide supplementary context information to support the Pre-Authorization.
- Both providers and patients should have access to more information on claims status.
Pre-authorization Improvement Initiatives
The Fast PATH Program Initiative for Pre-Authorization
A new program initiative called the Fast Prior Authorization Technology Highway (Fast PATH) was launched by America’s Health Insurance Plans (AHIP), along with several of the organization’s member insurance providers, to improve the pre-authorization process.
Prescribed Medication Pre-Auth Process
With the help of Surescripts technology, the most important clinical information will be made available to the doctors while the patient is still dealing with and getting informed about the prescribing process. A simpler, smoother process at the pharmacy counter will help the patient receive and take the medication quicker and easier.
Medical and Surgical Procedures Pre-Auth Process
Using Availity technology, physicians can access a multi-payer portal to simplify pre-authorization requests and approvals that may be required for different procedures. The multi-payer portal allows for easier communication, faster approvals, and quick turnaround, which in turn helps to speed up the delivery of quality patient care.
Automation & Digitalization of Pre-Auth Process
Automating digitizing the pre-authorization process can provide benefits including coordinated care, fewer claim denials, minimized healthcare costs, and quick decision-making from payers. This will ultimately support the transition to value-based care.
With each upcoming year into healthcare, more importance and highlights have been given to improve the quality of care given to patients and more regulations to incentivize the physicians so that they focus more on giving value-based care to members.
When physicians focus more on value-based, quality care, insurance payers can reduce the restrictions imposed on pre-authorizations. This can also help reduce the utilization of resources and time required to respond to requests.
A few of the steps that have been taken or are about to be taken for the digitization of the Pre-Auth process are described below:
| Solution Category | Solution Element | Benefits |
| Real-time and automated pre-auth | Real-time UI for providers to submit request / Get response to pre-auth (using TPA solutions like Availity and Emdeon). | Quick approval and response time with real-time transactions happening between providers and payers. |
| Using EDI 278 transaction requests to send in real-time and in batches. | Standardized and HIPAA-compliant transactions would help in streamlining prior authorization approvals. | |
| Auto-population of the Patient, Provider, Procedure, and medical treatment details in the filling system. | A more customer-centered approach for pre-authorization requests can reduce errors and delays. | |
| Digitalization | Artificial Intelligence (AI) for patient access workflow. | Streamlines the patient access workflow, which in turn helps in getting earlier approval for pre-authorizations. |
| Machine Learning (ML) for procedures/services prediction. | Helps in predicting procedures and services required by patients and thus enables doctors to commence the process of pre-authorization in advance. It learns from EHR patient data and develops predictions by identifying hidden patterns. | |
| Robotic Process Automation (RPA) for manual business processes | Provides a free platform that utilizes bots in automating manual business processes that take more hours and effort but do not require higher-level thinking. |
The Market for Pre-Authorization Automation Solutions
The pre-authorization request, response, and approvals processes are typically manual and time-consuming for physicians. This places a burden on insurance players to be compliant with high-value, quality care in less time.
Tech giants and health IT vendors of all sizes foresee the value and revenue earning opportunities inherent to using technological solutions to create a more efficient workflow. Giving insurance players and providers a streamlined, efficient, and less time-consuming process will benefit all.
Here are a few examples of what’s already happening in the space:
- Deloitte, in collaboration with NCT ventures, provides a cloud-based platform that helps in integrating and centralizing the process in hospitals, with health insurers able to check members’ eligibility and whether certain drugs are covered.
- Epic Systems, along with startup Klara, will provide the clinical messaging platform that improves communication between patients, their physicians, and insurers.
- ZappRx, a mid-sized US-based company, provides a comprehensive digital solution for physicians for specialty prescribing, referrals, and pre-authorization requests. The ZappRx platform can improve the physician prescription approval rate from weeks to just a few days, even for most complex cases.
- CenterX offers pre-authorization solutions along with its product offering of medication adherence components. The solution helps doctors be aware of out-of-pocket costs so that patients have the correct information in advance for their prescription therapy plan.
- Infinx provides a platform to receive faster Pre-Auth approvals using AI-driven technology plus certified specialists.
- Tech giant Apple proposed an iWallet that seamlessly connects providers and payers to assist in seamless referrals and pre-authorizations.
Conclusions
Streamlined, efficient, and real-time interactions will reduce the time spent on pre-authorization tasks for both payers and providers. Reducing delays and increasing staff productivity can then lead to timelier delivery of patient care.
A customer-centric process with refined and precise automated processes can only be achieved with new digital technologies that are regulated in keeping with the latest protocols and criteria.
Reference Links
Top Insights
If You Build Products, You Should Be Using...
Digital TransformationTesting and QAManufacturing and IndustrialPredictive Hiring (Or How to Make an Offer...
Project ManagementTop Authors
Blog Categories

Let’s Work Together
Related Content
Unlock the Power of the Intelligent Healthcare Ecosystem
Welcome to the future of healthcare The healthcare industry is on the cusp of a revolutionary transformation. As we move beyond digital connectivity and data integration, the next decade will be defined by the emergence of the Intelligent Healthcare Ecosystem. This is more than a technological shift—it's a fundamental change in how we deliver, experience, … Continue reading Digitalize Pre-Authorization Process →
Learn More
Leveraging SaMD Applications to Improve Patient Care and Reduce Costs
One of the most exciting developments in healthcare is the emergence of Software as a Medical Device (SaMD) as a more convenient and cost-effective means to deliver superior care to the tens of millions of people worldwide who suffer from various health conditions.
Learn More
If You Build Products, You Should Be Using Digital Twins
Digital twin technology is one of the fastest growing concepts of Industry 4.0. In the simplest terms, a digital twin is a virtual replica of a real-world object that is run in a simulation environment to test its performance and efficacy
Learn More
Share this page:
-
-
-
-
URL copied!