-
-
-
-
URL copied!
Data collected from users is essential for healthcare technology, but merely collecting this information is not enough. Attempting to achieve interoperability for complex health data and finding the easiest ways to improve interoperability in healthcare are undoubtedly the most significant next steps. Still, there are some challenges along the way.
Apart from complying with the three major components of the Health Insurance Portability and Accountability Act (HIPAA) law, interoperability in healthcare is complicated by hundreds of certified Electronic Health Records (EHRs) throughout the healthcare sector, each with distinct features, terminologies, and capabilities.
A further concern is the fact that many healthcare incumbents are supporting the status quo with data siloed into disparate systems, even though this approach may result in a deliberate blocking of information or the development of EHR systems with limited capabilities. Nonetheless, the proposed Fast Healthcare Interoperability Resources (FHIR) regulations promote innovation, interoperability, and the free flow of data in an effort to address such challenges.
To experience real innovation in the healthcare ecosystem, healthcare providers must embrace interoperable systems and open up data flow between them. For this to happen, all stakeholders must be committed to interoperability by taking steps to develop innovative products and solutions.
Finally, all stakeholders in the Health Tech industry should have a documented plan for improving the exchange of health data. In this context, we would like to discuss the following five most relevant aspects that health system leaders should consider when developing a documented plan on how to improve interoperability in healthcare:
Table of Contents
- 5 Basic Recommendations on How to Improve Interoperability in Healthcare
- Analyze the Interoperability Status of Healthcare Providers
- Understand Data Accessibility from the Inside Out
- Establish Proactive Collaborations Between Different Providers, Vendors, and the Staff
- Prioritize Data Security to Improve Healthcare Interoperability
- Continuously Train Staff on Healthcare Interoperability Improvements
- Conclusion
5 Basic Recommendations on How to Improve Interoperability in Healthcare
1. Analyze the Interoperability Status of Healthcare Providers
In light of the newly established standards regarding interoperability and the levels of interoperability in healthcare, new challenges become more apparent when organizations or vendors are not aligned with regard to enacting FHIR standards. Misalignments in the past prevented healthcare tech vendors from accessing and integrating critical data. It should no longer be the case, or at least not because of technological limitations.
To make a significant impact, healthcare tech teams must assess how hospitals and practices perform in terms of interoperability. Major EHR and Electronic Medical Records (EMR) systems previously closed are now beginning to open. It is essential to understand how to implement changes following industry standards to avoid wasting these innovations.
Overall, the process of improving interoperability in healthcare may take time, as an organization decides how to best implement FHIR, SMART on FHIR, servers, or just mandatory requirements. Still, more organizations will likely embrace these standards.
2. Understand Data Accessibility from the Inside Out
The most recent updates to the Final Rule Policy emphasize the importance of standardized APIs for the health sector. Ultimately, it will make it feasible for various systems to communicate seamlessly and empower individuals with secure access to health information through mobile phones and other digital devices.
In this regard, one of the most significant challenges facing healthcare tech vendors is that they are unaware of what data is available to them, whether it is from a source system or not, what that data means, or where it is located. Therefore, organizations must define what type of data they have, what data they intend to exchange, where they must transmit it, and how the recipient systems will use it before exchanging data.
By defining the data lifecycle, healthcare software development companies can establish appropriate standards and understand what needs to be done to make data meaningful.
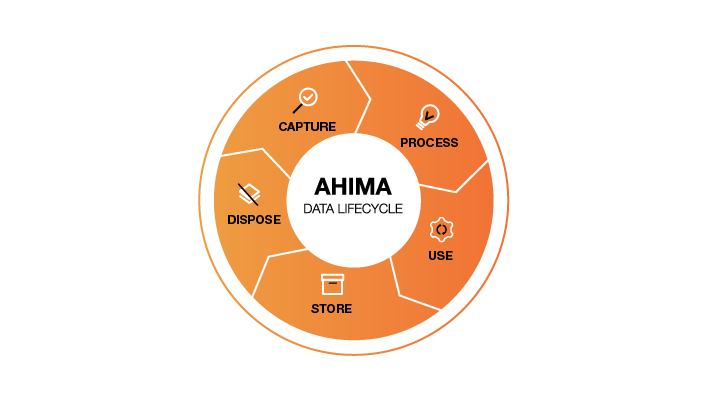
Source: Healthcare Data Governance Brief – The American Health Information Management Association, 2022
The leaders of health systems must also identify the data elements that need to be shared with patients and third parties, be it for data collection or reporting. After identifying the data, the next step would be identifying gaps in the data collection that should be documented.
As healthcare vendors are responsible for producing high-quality and easily understandable patient records for doctors, staff, and patients, this is a critical consideration in improving interoperability in healthcare.
3. Establish Proactive Collaborations Between Different Providers, Vendors, and Staff
To improve EHR usability and interoperability in the healthcare industry, a close and transparent collaboration between vendors and healthcare organizations is essential.
This applies not only to the implementation stage but also to ensuring interoperability. Imagine a primary care practice needing to enter EHR data and extract data accurately and efficiently to generate quality measures and other metrics. Currently, most EHRs do not provide the ability to generate reports that would assist medical practices in improving the quality of patient care from this perspective.
This is the result of several factors.
A major challenge is the fact that multiple EHRs used by different healthcare providers for the same patient do not communicate with one another. Due to the differences between the sites of care and the EHRs, a patient’s lab results from a month ago may be available, but those from a week ago may not be. As a result, confusion, errors, and delays may result in care delivery.
What matters most is ensuring that the teams across health technology systems have developed an effective method for integrating EHR data. The approach should be viewed as one more step in improving care delivery and patient outcomes, and it must be based entirely on a collaborative approach.
4. Prioritize Data Security to Improve Healthcare Interoperability
There is no doubt that data security is of the utmost importance in the healthcare industry. Rather than disregard past situations in which healthcare data was the subject of many cybersecurity threats and attacks, leading to severe losses for some stakeholders, it is a matter of learning from them. The absence of a 360-degree security system can also hinder the security of vulnerable information concerning patient records. In turn, this can result in situations where a patient’s life is at risk.
To achieve interoperability, security should be at the forefront of the development process. This means that stakeholders in healthcare should trust one another and find a viable way to align health systems and health plans. This will enable them to eventually develop the trust that most patients seek regarding healthcare information exchange.
Data security may appear challenging to achieve at a high level, but it is a mandatory requirement and certainly not impossible. Healthcare organizations in the United States have an advantage in complying with security regulations such as HIPAA since they have to work with service providers who can assist them in understanding and adhering to these regulations.
A secure API approach to improving interoperability in healthcare will enable your system to become a robust health IT system that places quality of care at the forefront of its design. Teams with a well-balanced set of skills are crucial to developing a secure system that will be interoperable with the overall healthcare ecosystem and considering the user experience as a key component.
5. Continuously Train Staff on Healthcare Interoperability Improvements
Upgrading systems or implementing improvements successfully can sometimes require more involvement from healthcare providers than we might expect.
For example, when improving the interoperability in healthcare and developing new integrations, those using the system must thoroughly understand it to use it effectively. Therefore, the organization must provide continuous training and education about the new approach to employees in collaboration with the health technology vendors responsible for the upgrade.
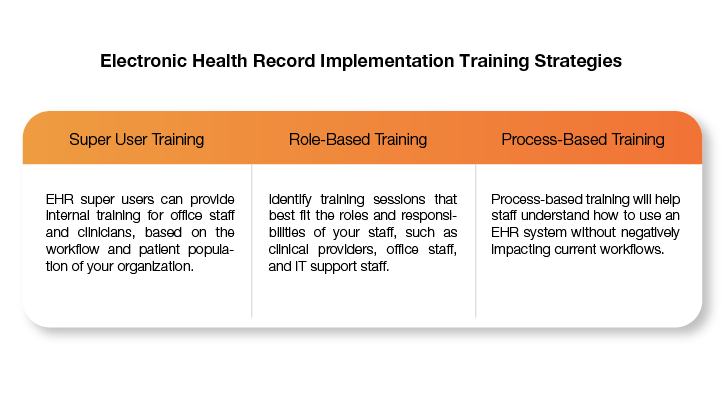
Source: HealthIT.gov
Engaging staff while improving current systems will ensure smooth use of these changes and allow them to better understand where they will benefit from them. In the case of interoperability in healthcare, ensuring that medical staff is familiar with ICT tools will allow them to retrieve and communicate necessary information as needed. This will enable them to reduce unnecessary workloads, convert to digital systems, and provide better documentation of patient activity.
Ultimately, training medical staff is an essential investment for improving interoperability in healthcare, resulting in straightforward health information exchanges (past medical history, laboratory orders & results, patient referrals, discharge summaries, etc.) for healthcare providers
Conclusion
Despite the progress made in interoperability, there is still room for improvement. In the past, healthcare interoperability has primarily dealt with helping healthcare facilities exchange data across borders, but in the future, health data transmission and consumption will become more standardized.
Interoperability between the systems of different organizations will allow data to be shared across organizations instead of remaining isolated within one provider. After determining how to improve interoperability in healthcare, systems can be connected more efficiently, and EHRs can connect to other applications and connected devices through standards of APIs.
As shown, it is possible to improve interoperability in healthcare when system integrations and implementations are carefully planned. Taking aspects like those discussed in this article into account may enable your organization to reap the benefits of healthcare interoperability, which may impact healthcare innovation.
With the help of experienced healthcare software development teams having interdisciplinary skills and extensive knowledge, you will be able to speed up the development of interoperable healthcare software. Intensifying valuable and secure innovations can only be achieved through alignment. This is why it’s important to have an upfront conversation with your future tech partner to determine if you are compatible.

Let’s Work Together
Related Content
Unlock the Power of the Intelligent Healthcare Ecosystem
Welcome to the future of healthcare The healthcare industry is on the cusp of a revolutionary transformation. As we move beyond digital connectivity and data integration, the next decade will be defined by the emergence of the Intelligent Healthcare Ecosystem. This is more than a technological shift—it's a fundamental change in how we deliver, experience, … Continue reading Recommendations on How to Improve Interoperability in Healthcare →
Learn More
Crowd-Striked: Lessons Learned and Best Practices for Future Prevention
Incident Summary On July 19, 2024, CrowdStrike released a content configuration update for the Windows sensor that resulted in widespread system instability, causing Windows systems to experience the "Blue Screen of Death" (BSOD). The issue was traced to a channel file named “C-00000291*.sys” included in the update, which caused system crashes upon deployment. “Channel files” … Continue reading Recommendations on How to Improve Interoperability in Healthcare →
Learn More
Share this page:
-
-
-
-
URL copied!